In recent years, substance abuse has risen to epidemic proportions in the U.S., according to several studies, one of which comes from the National Institutes of Health (NIH). In that study, George F. Koob, Ph.D., an esteemed expert on alcohol, stress, and the neurobiology of alcohol and drug addiction, revealed that an estimated 23 million adults in the U.S. have previously or currently struggle with a substance abuse problem. The same study further revealed only 10% of Americans with a substance abuse problem ever receive the treatment necessary to turn their lives around. In a separate study from the Centers for Disease Control and Prevention (CDC), researchers revealed that over 100,000 Americans died from a drug overdose in 2021, an increase of roughly 28% over the nearly 79,000 overdose deaths reported in 2020. It is worth noting that both studies show that substance abuse, in all of its many forms, is costing the U.S. economy more than $600 billion annually. One of the drugs costing the U.S. economy a king’s ransom is Fentanyl, a synthetic opioid that accounted for an astonishing 68% of all drug overdose deaths in 2019.
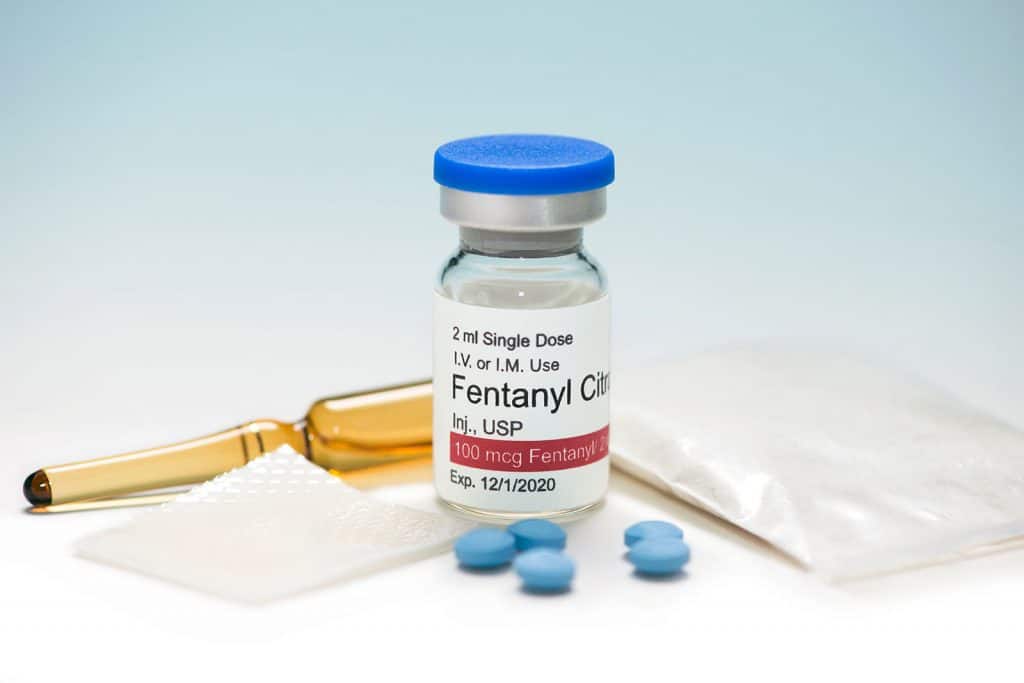
What Is Fentanyl?
In many ways, Fentanyl is a lot like OxyContin, Morphine, and Hydrocodone in that it is a powerful and highly addictive opioid. But it is far more powerful and even more addictive than these drugs. For this reason, most physicians only prescribe it as a last resort for treating chronic and severe pain. Most of the time, they will prescribe it to cancer patients or patients that have become tolerant of less powerful opioid drugs, such as OxyContin, Morphine, and Hydrocodone. Some 50 to 100 times stronger than morphine, Fentanyl is available in several forms, including transdermal patches, lozenges, nasal sprays, tablets, and injectables. Unlike other opioid drugs derived from the opium poppy plant, legal Fentanyl is made in state-of-the-art labs by scientists using the same chemical structure used to make opioids derived from poppy plants. Illegal Fentanyl, on the other hand, is made in less-than-ideal environments by untrained and unlicensed individuals.
How Does Fentanyl Work?
The way Fentanyl works when it comes to relieving pain is not too dissimilar from how other opioid drugs work. When someone takes this powerful, synthetic opioid, it binds to receptors in the areas of the brain responsible for regulating pain and emotions. The benefit here is twofold; the drug interacts with the prefrontal cortex in the brain, which alters how the body perceives and responds to pain. It also triggers intense feelings of euphoria by boosting dopamine levels in the brain, which further helps to keep pain under control. But there is a downside insofar as the same intense euphoria brought on by Fentanyl is the very thing that drives many people to misuse, abuse, and, ultimately, become addicted to the drug. Of course, most don’t realize that they are addicted to this powerful, synthetic opioid until they abruptly stop taking it and are met with a whirlwind of unpleasant symptoms. Some of these symptoms include the following:
- Drowsiness
- Confusion
- Dizziness
- Nausea and vomiting
- Constricted pupils
- Urinary retention and constipation
- Respiratory depression
To get some much-needed relief from these symptoms and to enjoy the blissful euphoria they’ve grown accustomed to, most people will do whatever it takes to get their hands on more Fentanyl. And they continue to do so until they either get help to overcome their addiction or suffer a fatal overdose, which can very well happen if they take too much of the drug. Some of the symptoms synonymous with a Fentanyl overdose include
- Hypotension
- Dizziness and drowsiness
- Nausea and vomiting
- Feeling limp
- Cold or clammy skin
- Cyanosis
- Changes in breathing
- Foaming at the mouth
- Bradycardia
- Reduced or loss of consciousness
- Coma
Fortunately, many of the over 3 million people in the U.S. who have a problem with Fentanyl and other opioids are going to rehab facilities to get the help they need to overcome addiction. And it is safe to say they made the right choice since quitting opioids without professional help is not easy.
The Reality of Going Through a Fentanyl Detox
The human body naturally works to rid itself of Fentanyl and other harmful contaminants once an individual stops taking it, a process known as detox. And it will continue this process until the body is free of Fentanyl and any associated contaminants. Although this is a critical step toward ending one’s relationship with Fentanyl, it is not easy as it can trigger the kind of withdrawal symptoms discussed earlier in this article. Mindful of just how challenging this aspect of addiction recovery can be for most people, most rehabs in the U.S. offer medication-assisted detox.
Why Medication-Assisted Detox Is the Right Choice When Trying to Quit Fentanyl
Studies show as much as 91% of people fall victim to relapse while detoxing from Fentanyl, with the vast majority citing the inability to cope with severe withdrawal symptoms as the primary reason. The benefit of medication-assisted detox is that it lowers an individual’s chance of relapse by providing much-needed relief from severe withdrawal symptoms that would otherwise lead to them using again when they want nothing more than to quit Fentanyl for good. The medications that many physicians prescribe to individuals as part of a medication-assisted detox program include Methadone, Suboxone, Naltrexone, and the newly-approved Lucemyra. It is worth noting that medication-assisted detox also includes round-the-clock monitoring by a licensed physician or nurse, which can prove invaluable should an individual start to struggle with life-threatening withdrawal symptoms, such as coma, for example. This addiction recovery treatment, which many describe as a godsend, is generally offered until an individual completes detox.
How Long Does Fentanyl Stay In Your System?
Having established that detox is one of the more challenging parts of overcoming an addiction to Fentanyl and that it continues until the drug is out of one’s system, let’s shift gears and discuss how long it takes the body to get rid of it completely. Detoxing from Fentanyl can take anywhere from 5 to 10 days. However, this does not mean the body is 100% free of the drug. This timeframe only refers to how long it will take for someone to achieve relief from severe fentanyl withdrawal symptoms naturally. The complete timeline when it comes to how long it will take the body to rid itself of Fentanyl is as follows:
- 24 to 72 hours to no longer show up in urine
- 5 to 48 hours to no longer show up in the blood
- Up to 3 months to no longer show up in hair
How long Fentanyl stays in one’s system depends on whether we are talking about in someone’s urine, blood, or hair. It also depends on whether we’re talking about achieving relief from severe withdrawal symptoms or merely passing a drug test.
Bottom Line
In summary, Fentanyl is a powerful synthetic opioid that does a remarkable job in terms of providing relief from chronic pain. But people can become physically and psychologically addicted to it if they misuse or abuse it. And it takes getting through several nightmarish withdrawal symptoms before someone can overcome a Fentanyl addiction. The same applies to it showing up in a drug test.
FAQ
How does fentanyl make you feel?
How long do pain pills stay in your system?
How long does Fentanyl stay in urine?