Anxiety is a common mental illness that causes people to worry too much, dread too much and have hypersensitive bodies. It permeates every aspect of life, from relationships to general health, and goes well beyond causing only emotional misery. Anxiety, if untreated, may have negative effects on one’s physical health, social relationships and overall quality of life. It can interfere with everyday functioning, impede personal and professional development and even lead to the onset of other mental health conditions. In order to get back on track and create a better, more satisfying life for oneself, it is crucial to get treatment as soon as possible. But not all treatments are the same. Some are very addictive, like Xanax, which can exacerbate anxiety. Fortunately, there are several non-additive alternatives.

What Is Xanax?
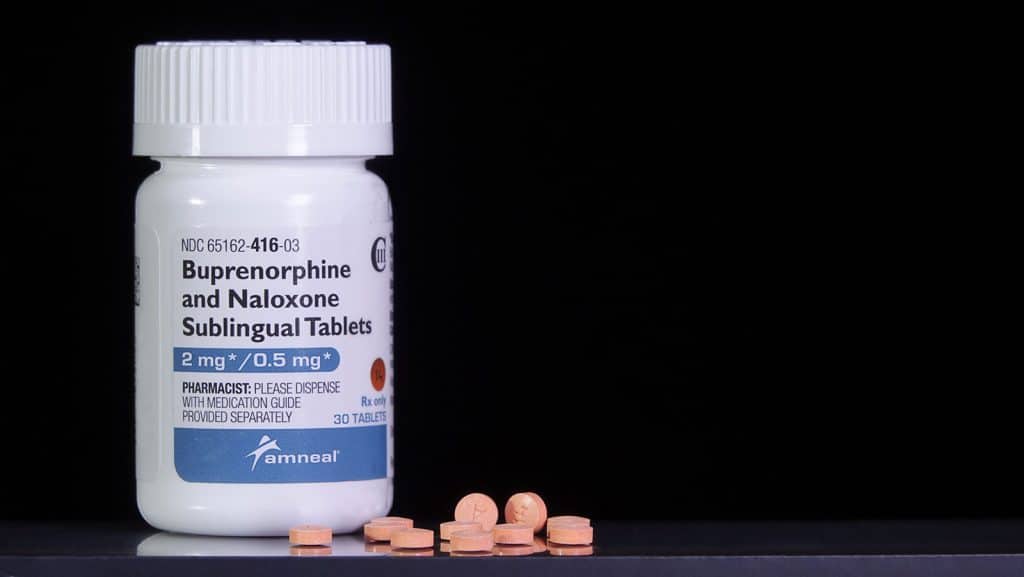
Xanax is a benzodiazepine that commonly goes by the name alprazolam. It operates in the brain by amplifying GABA’s inhibitory effects. As a result of lower neuronal activity, GABA induces a calming effect.
Since Xanax takes effect quickly, it is mainly given to patients suffering from anxiety and panic disorders. It provides rapid relief during periods of elevated anxiety. However, some doctors may prescribe it for short-term use to treat acute symptoms of anxiety.
Xanax is an effective anxiety medication, but it comes with serious hazards, including dependency and withdrawal. This is why physicians are typically very hesitant about prescribing it. Instead, they look into other options for long-term anxiety management.
Addiction Rate of Xanax and Withdrawal Symptoms
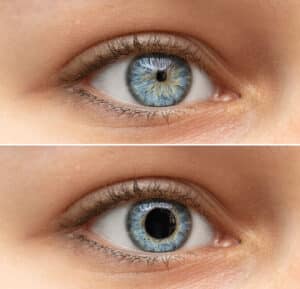
A report published in 2019 stated that 30.6 million adults in America used benzodiazepines. 17.2% of those people reported misusing the drug. That’s 5,263,200 people. Those addicted to Xanax often experience a number of withdrawal symptoms, which may include:
- anxiety
- panic attacks
- loss of appetite
- abnormal sensations
- hyperventilation
- sensitivity to light or sound
- tremors
- sweating
- muscle spasms
- seizures
- psychosis
- sleep problems
Xanax Addiction Treatment Options
There are benefits and drawbacks to the various approaches used by treatment providers to combat Xanax addiction. One way to control withdrawal symptoms is by gradually weaning off the drug under medical supervision. It also helps to take part in treatments that target the underlying reasons for addiction, such as cognitive-behavioral therapy.

It is important to note that each therapy handles Xanax addiction in its own unique way, emphasizing the necessity for personalized treatment strategies. Support groups can provide a feeling of belonging and empathy, but they might not be able to meet your specific needs. And even though inpatient rehabilitation offers extensive treatment, it can sometimes interfere with normal activities. Flexibility is key in outpatient programs, but self-discipline is essential.Non-Addictive Alternatives to Xanax
Due to its addictive properties, Xanax carries the danger of both physical dependence and withdrawal. Non-addictive solutions provide excellent treatment without the risks of addiction, making it easier to sustain long-term control over your anxiety.
SNRIs
The antidepressant medication family known as SNRIs (serotonin-norepinephrine reuptake inhibitors) works by increasing brain levels of the neurotransmitters serotonin and norepinephrine. With their slow onset of action, SNRIs provide effective treatment without the risk of addiction associated with benzodiazepines, in contrast to Xanax. By controlling neurotransmitters, these non-addictive anxiety medications improve mood and lessen anxiety, making them useful as long-term treatments.
SSRIs
Antidepressants known as SSRIs (Selective Serotonin Reuptake Inhibitors) work by increasing the brain’s serotonin levels. In contrast to Xanax, SSRIs provide a steady improvement in mood by slowly preventing the absorption of serotonin. They are a better option than benzodiazepines since they alleviate anxiety without the common side effects of withdrawal and dependency.
Buspirone
Buspirone, an anxiolytic (anxiety-reducing) drug, has a less severe effect on the central nervous system than Xanax since it interacts with serotonin receptors. The full effects of buspirone do not occur for many weeks because of its delayed start. It provides anxiety alleviation without the dangers of addiction or withdrawal due to its non-addictive nature. For those looking for a non-addictive option for long-term usage, Buspirone is a good substitute for Xanax since it offers consistent and long-lasting anxiety relief.
Beta-Blockers
Although beta-blockers are primarily used to treat hypertension and cardiac problems, they have recently attracted interest for their potential off-label usage in the treatment of anxiety. Beta-blockers are a class of drugs that work by preventing the heart from responding to adrenaline. Benzodiazepines like Xanax have an effect on the brain’s neurotransmitters, whereas beta-blockers don’t. On the contrary, they alleviate the bodily manifestations of worry, such as a high heart rate and shakiness. Because of this, they are a safer option than Xanax.
Hydroxyzine
The anxiolytic qualities of the antihistamine hydroxyzine make it a common anti-anxiety medication choice. Hydroxyzine affects the central nervous system by inhibiting histamine receptors, unlike the benzodiazepine Xanax. Instead of affecting neurotransmitters directly, as Xanax does, this viable substitute aids in the management of anxiety symptoms without the risk of addiction.
Valerian Root
Famous for its sedative effects, the Valeriana officinalis plant is the source of the herbal supplement known as valerian root. Because of its ability to interact with the GABA receptors in the brain, valerian root serves as a non-addictive substitute for the benzodiazepine Xanax. There are also no side effects or dependencies associated with valerian root, which is unlike Xanax. Common uses include managing stress, getting a better night’s sleep and reducing anxiety.
Conclusion
Although Xanax is beneficial for short-term anxiety treatment, it is highly addictive. When it comes to managing anxiety, you have a variety of non-addictive alternatives to choose from. No matter which types you use, always speak with a physician or healthcare professional to determine the most suitable option based on your individual needs and medical history.
To learn more about safely using Xanax alternatives, contact Garden State Detox now.